Ibrutinib (Imbruvica) has "become for many clinicians the treatment of choice" for patients with relapsed or refractory Waldenstrom macroglobulinemia (WM). This class of agents (Bruton tyrosine kinase [BTK] inhibitors) represents a "paradigm shift" for the treatment of this disease, says Roger Owen, MD, the St. James Institute of Oncology, Leeds, United Kingdom.
He was commenting in an editorial published online January 14 in the Journal of Clinical Oncology. His editorial was prompted by the publication of final, longer-term results from a pivotal study of the drug.
These longer-term results have now established ibrutinib as one of the most effective monotherapies for WM, say the trialists who conducted the pivotal study.
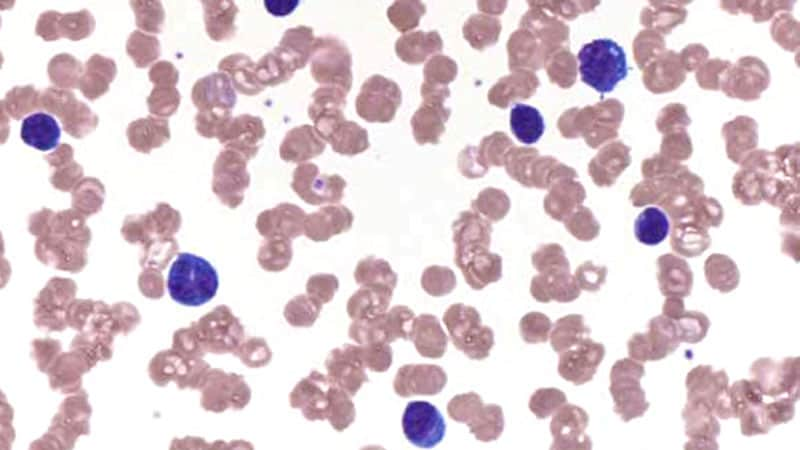
Ibrutinib was used in the treatment of 63 patients with symptomatic, relapsed, or refractory WM. At a median follow-up of 59 months, the overall response rate to ibrutinib monotherapy was 90.5%. The major response rate was 79.4% with deepening responses. The rate of very good partial response (VGPR) increased to 30.2% over time, say Steven Treon, MD, PhD, the Bing Center for Waldenstom's Macroglobulinemia, Dana-Farber Cancer Institute, Boston, Massachusetts, and colleagues.
Their findings were published online September 15, 2020, in the Journal of Clinical Oncology.
These mature data clearly demonstrate "real clinical benefit for patients," comments Owen in his editorial.
This pivotal study led to approval of ibrutinib for the treatment of relapsed or refractory WM in 2015. The drug become the first therapeutic agent to be approved by the US Food and Drug Administration for this disease.
"Interestingly, the regulatory approval also permitted its use in previously untreated patients if they were considered unsuitable or unfit for rituximab-based therapies," he adds.
Longer PFS Than Seen With Other Drugs
The pivotal study by Treon and colleages involved 63 patients who had previously undergone treatment with a median of two therapies (range, one to nine therapies). For approximately 40% of the patients, disease was refractory to previous therapy.
All patients received ibrutinib at a dose of 420 mg daily, but dose reductions were permitted if unacceptable toxicity developed.
"Patients received ibrutinib on study for 40 months and thereafter," explain Treon and colleagues. A total of 36 patients completed the long-term follow-up study.
Responses were judged by a decrease in immunoglobulin M (IgM) level; a decrease of 25% to 49% was considered a minor response (MR); a decrease of 50% to 89%, a partial response (PR); and 90% or greater, a VGPR. "The overall response rate included MR or better and major response rate included PR or better," they explain.
Median serum IgM levels declined from 3520 mg/dL to 821 mg/dL at best response (P < .001). For 41% of the cohort, the serum IgM level was in excess of 4000 mg/dL prior to their receiving irbrutinib; at best response after treatment, in only one patient did serum IgM exceed 4000 mg/dL (P < .001).
Median bone marrow involvement dropped from 60% before treatment to 20% after treatment (P < .001). Hemoglobin increased from a median of 10.3 g/dL prior to treatment to 14.2 g/dL after treatment (P < .001). The authors point out that anemia is the most common morbidity among patients with WM.
However, the researchers caution that "overall and major response rates were impacted by MYD88 and CXCR4 mutation status." The presence of both MYD88 and CXCR4 wild-type disease is associated with very poor overall, major, and VGPR rates.
In the group overall, there were no complete responses (CRs), so mutational status did not affect CR rates.
Table. Response Rates (RR) by Mutational Status
| All | MYD88 mutated, CxCR4 wild type | MYD88 mutated, CxCR4 mutated | MYD88 wild type, CXCR4 wild type | P value | |
|---|---|---|---|---|---|
| Number of patients | 63 | 36 | 22 | 4 | |
| Overall RR | 90.5% | 100% | 86.4% | 50.0% | <.0100 |
| Major RR | 79.4% | 97.2% | 68.2% | 0% | <.0001 |
| No response | 9.5% | 0% | 13.6% | 50% | <.001 |
| VGPR | 30.2% | 47.2% | 9.1% | 0% |
The 5-year progression-free survival (PFS) rate for all patients was 54%. Again, MYD88 and CXCR4 mutational status affected PFS.
For example, median PFS was not reached by study endpoint for patients with MYD88-mutated disease and CXCR4 wild-type disease. For these patients, PFS at 5 years was 70%.
In contrast, for patients with both MYD88- and CXCR4-mutated disease, the median PFS at 5 years was 38%. Among patients with CXCR4-mutated disease, the 5-year PFS rate was 50%.
Prognosis was worse for patients who had both MYD88 and CXCR4 wild-type disease. All of these patients experienced disease progression within 2 years of treatment.
The long durability of the median PFS produced by single-agent ibrutinib in this patient population is superior to that achieved with any other agent or combination of agents and is on par with median PFS following autologous transplant, the authors comment.
Adverse events (AEs) of grade 3 or higher that were possibly related to ibrutinib included neutropenia (about 16%), thrombocytopenia (about 11%), and pneumonia (about 3%).
Five patients discontinued treatment because of AEs. The researchers conclude, "[These] findings provide a cogent case for the preferred use of ibrutinib in most previously treated patients who are BTK inhibitor naive." They emphasize that "the sustained long-term control of disease in the absence of a CR supports the notion that attainment of CR need not be the primary goal of therapy in WM."
Questions to Be Explored
In his editorial, Owen suggests a number of questions that should be investigated in further studies.
Should all patients with relapsed WM receive ibrutinib? Should ibrutinib now be considered for all treatment-naive patients, regardless of comorbidities and performance status? Importantly, how should patients with MYD88 wild-type disease be managed, and can physicians use mutational status to optimize treatment?
Furthermore, do either second-generation BTK inhibitors or combinations of different agents further improve efficacy? Rational chemotherapy-free combinations should be evaluated, because a potentially curative treatment for WM is now a realistic goal, he comments.
The study was funded by Pharmacyclics. Treon has served as a consultant or in an advisory role for Janssen Pharmaceuticals, Pharmacyclics, BeiGene, X4 Pharmaceuticals, and Bristol-Myers Squib. Owen has received honoraria from Janssen-Cilag, BeiGene, Celgene, and AstraZeneca and has served as a consultant or as an advisor to BeiGene and Janssen-Cilag.
J Clin Oncol. Published September 15, 2020. Full text, Editorial
For more from Medscape Oncology, join us on Twitter and Facebook.
"choice" - Google News
January 28, 2021 at 01:27AM
https://ift.tt/3t2lDm3
Ibrutinib 'Treatment of Choice' in Waldenstrom Macroglobulinemia - Medscape
"choice" - Google News
https://ift.tt/2WiOHpU
https://ift.tt/3c9nRHD
Bagikan Berita Ini














0 Response to "Ibrutinib 'Treatment of Choice' in Waldenstrom Macroglobulinemia - Medscape"
Post a Comment